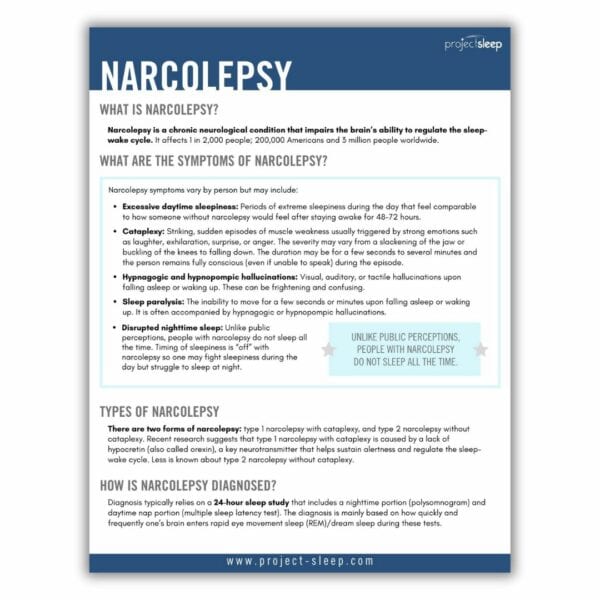
Narcolepsy is a chronic neurological condition that impairs the brain’s ability to regulate the sleep-wake cycle. It affects 1 in 2,000 people; 200,000 Americans and 3 million people worldwide.
Narcolepsy
What are the symptoms of narcolepsy?
Narcolepsy symptoms vary by person but may include:
- Excessive daytime sleepiness: Periods of extreme sleepiness during the day that feel comparable to how someone without narcolepsy would feel after staying awake for 48-72 hours.
- Cataplexy: Striking, sudden episodes of muscle weakness usually triggered by strong emotions such as laughter, exhilaration, surprise, or anger. The severity may vary from a slackening of the jaw or buckling of the knees to falling down. The duration may be for a few seconds to several minutes and the person remains fully conscious (even if unable to speak) during the episode.
- Hypnagogic and hypnopompic hallucinations: Visual, auditory, or tactile hallucinations upon falling asleep or waking up. These can be frightening and confusing.
- Sleep paralysis: The inability to move for a few seconds or minutes upon falling asleep or waking up. It is often accompanied by hypnagogic or hypnopompic hallucinations.
- Disrupted nighttime sleep: Unlike public perceptions, people with narcolepsy do not sleep all the time. Timing of sleepiness is “off” with narcolepsy so one may fight sleepiness during the day but struggle to sleep at night.
Types of narcolepsy
There are two forms of narcolepsy: type 1 narcolepsy with cataplexy, and type 2 narcolepsy without cataplexy. Recent research suggests that type 1 narcolepsy with cataplexy is caused by a lack of hypocretin (also called orexin), a key neurotransmitter that helps sustain alertness and regulate the sleep-wake cycle. Less is known about type 2 narcolepsy without cataplexy.
How is narcolepsy diagnosed?
Seeing a sleep specialist is recommended for people who are experiencing symptoms that indicate you may be living with narcolepsy.
Diagnosis typically relies on a 24-hour sleep study that includes a nighttime portion (polysomnogram) and daytime nap portion (multiple sleep latency test). The diagnosis is mainly based on how quickly and frequently one’s brain enters rapid eye movement sleep (REM)/dream sleep during these tests.
How is narcolepsy treated?
There is currently no cure for narcolepsy. Treatment for symptom management varies widely by person and it often takes a long time to find the right combination of treatments.
Nighttime or histamine-directed medications can be used to decrease excessive daytime sleepiness and cataplexy.
Wake-promoting or stimulant medications can be used to increase alertness.
Antidepressant medication can be used to decrease cataplexy.
Scheduled daytime naps are an important part of treatment for many people.
Social support in the form of meet-up groups or on social media can help people with narcolepsy and their families to live well with narcolepsy.
Improvement in general health and wellness through sleep hygiene, diet, and fitness can help improve overall quality of life for people with narcolepsy.
Narcolepsy Awareness
Because of low awareness (even among physicians) and misperceptions, there is an average of 8 to 15 years between narcolepsy symptom onset and diagnosis. It’s estimated that the majority of people with narcolepsy are currently undiagnosed or misdiagnosed. Common misdiagnoses include epilepsy, depression, and schizophrenia.
If you suspect that you or a loved one could have narcolepsy, it is important to consult an AASM board-certified sleep medicine doctor. To find a local sleep specialist or accredited sleep center, visit www.sleepeducation.org.
Public misperceptions of narcolepsy lead to delayed diagnosis and treatment.
Additional Resources
For more information and resources, please visit Narcolepsy Network and Wake Up Narcolepsy. Please also download our free, printable Narcolepsy Fact Sheet for a handy resource to share with friends, family, and medical providers.
Narcolepsy Nerd Alert
The Narcolepsy Nerd Alert series invites fellow #NarcolepsyNerds to explore aspects of the narcolepsy experience, contemplate bold questions, and learn from each other.
Narcolepsy Nerd Alert: Living with Idiopathic Hypersomnia
Narcolepsy Nerd Alert: Could I Have Narcolepsy?
Rising Voices Stories: Narcolepsy
Project Sleep’s Rising Voices program serves the dual purpose of fostering a new generation of patient-advocates spreading awareness of sleep disorders while empowering participants.