Restless legs syndrome (RLS) or Willis-Ekbom disease is a neurological movement disorder that is often associated with a sleep complaint. People with RLS experience an almost irresistible urge to move their legs, usually due to disagreeable leg sensations that are worse during inactivity and often interfere with sleep.
Restless Legs Syndrome (RLS)
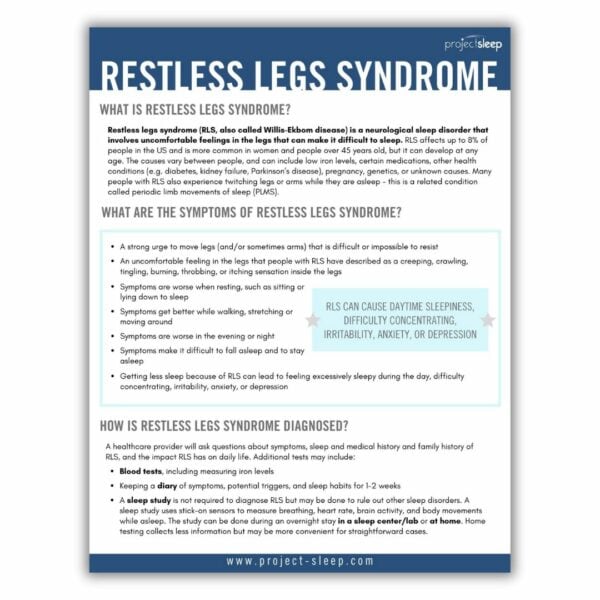
What is restless legs syndrome?
Restless legs syndrome (RLS, also called Willis-Ekbom disease) is a neurological sleep disorder that involves uncomfortable feelings in the legs that can make it difficult to sleep. RLS affects up to 8% of people in the US and is more common in women and people over 45 years old, but it can develop at any age.
The causes of RLS vary between people, and can include low iron levels, certain medications, other health conditions (e.g. diabetes, kidney failure, Parkinson’s disease), pregnancy, genetics, or unknown causes.
Many people with RLS also experience twitching legs or arms while they are asleep – this is a related condition called periodic limb movements of sleep (PLMS).
RLS affects up to 8% of people in the US.
What are the symptoms of restless leg syndrome?
- A strong urge to move legs (and/or sometimes arms) that is difficult or impossible to resist
- An uncomfortable feeling in the legs that people with RLS have described as a creeping, crawling, tingling, burning, throbbing, or itching sensation inside the legs.
- Symptoms are worse when resting, such as sitting or lying down to sleep
- Symptoms get better while walking, stretching, or moving around
- Symptoms are worse in the evening or night
- Symptoms make it difficult to fall asleep and to stay asleep
- Getting less sleep because of RLS can lead to feeling excessively sleepy during the day, difficulty concentrating, irritability, anxiety, or depression
How is restless legs syndrome diagnosed?
A healthcare provider will ask questions about your symptoms, sleep, and medical history and family history of RLS. They will also ask about the impact RLS has on your daily life. You may be asked to perform additional tests, such as:
- A blood test, including measuring iron levels
- Keeping a diary of symptoms, potential triggers, and sleep habits for 1-2 weeks
- A sleep study (polysomnography)
A sleep study is not required to diagnose RLS but may be done to rule out other sleep disorders. The study uses stick-on sensors to measure breathing, heart rate, brain activity, and body movements while asleep. It can be done during an overnight stay in a sleep center/lab or at home. Home testing collects less information but may be more convenient for straightforward cases.
How is restless legs syndrome treated?
It’s possible that other health issues may be causing a person’s RLS. Treating these issues may alleviate RLS symptoms.
Helpful strategies for coping with RLS and reducing its symptoms include:
- keeping healthy sleep habits
- getting moderate daily exercise
- eating well and avoiding caffeine, alcohol, and nicotine
Symptoms can also be relieved by moving or stretching legs, a hot bath, leg massage, and applying cold or hot packs.
Medications that increase dopamine levels in the brain are approved by the FDA for RLS, however these become less effective after using them for a while. Some medications typically used to treat seizures are also FDA-approved for RLS.
Research suggests that some medications that are FDA-approved for other conditions can be effective for RLS. Healthcare providers may prescribe these “off-label,” including opioids, which can be helpful for severe symptoms but can be habit-forming. Iron supplements may also be prescribed if iron/ferritin levels are low.
Social support from other people with RLS can help people manage their RLS.
Additional RLS Resources
Please download our free, printable RLS Fact Sheet for a handy resource to share with friends, family, and medical providers.