Insomnia is a chronic or acute sleep disorder. It is characterized by difficulty falling asleep, waking up frequently during the night, waking up too early, or feeling unrefreshed after waking.
Insomnia
What is insomnia?
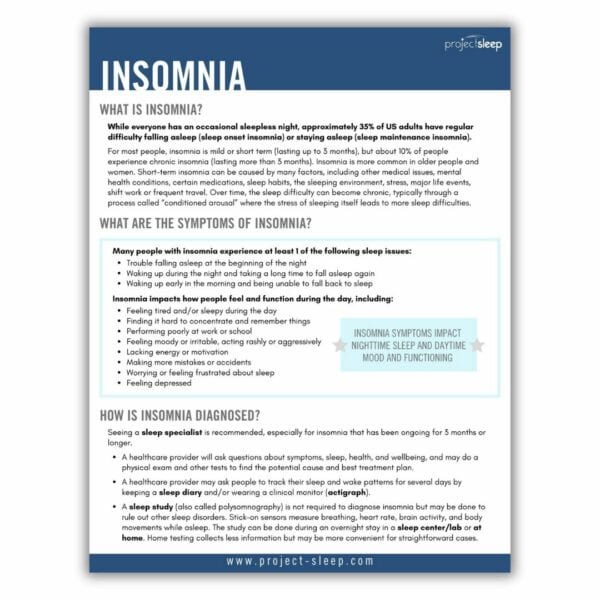
Although everyone has an occasional sleepless night, approximately 35% of US adults experience regular difficulty falling asleep or staying asleep. For most people, insomnia is mild or short term, lasting up to 3 months. About 10% of people experience chronic insomnia, lasting more than 3 months.
Short-term insomnia can be caused by many factors, including other medical issues, mental health conditions, certain medications, sleep habits, sleeping environment, stress, major life events, shift work, or frequent travel. Older people and women are also more likely to experience prolonged sleep difficulties.
Over time, the sleep difficulty can become chronic, typically through a process called “conditioned arousal” where the stress of sleeping itself leads to more sleep difficulties.
Approximately 35% of US adults experience regular difficulty falling asleep or staying asleep.
What are the symptoms of insomnia?
Many people with insomnia experience at least one of the following sleep issues:
- Trouble falling asleep at the beginning of the night
- Waking up during the night and taking a long time to fall asleep again
- Waking up early in the morning and being unable to fall back to sleep
Insomnia impacts how people feel and function during the day. Those experiencing sleep difficulties may feel tired and/or sleepy during the day. They might find it hard to concentrate and remember things, make more mistakes or accidents, and lack energy or motivation. These factors could cause poor performance at work or school.
It’s also common for people experiencing insomnia to feel moody or irritable, sometimes acting rashly or aggressively. Worrying or feeling frustrated about sleep is common, and there is an increased risk of depression.
How is insomnia diagnosed?
Seeing a sleep specialist is recommended, especially for insomnia that has been ongoing for 3 months or more.
A healthcare provider will ask questions about symptoms, sleep, health, and wellbeing. They may do a physical exam and other tests to find the potential cause and best treatment plan. Some providers may ask you to monitor your sleep and wake activity for several days by keeping a sleep diary or wearing a clinical device (e.g. an actigraph).
Though not required for diagnosis, an overnight sleep study (polysomnography) may help to rule out other sleep disorders. Stick-on sensors measure breathing, heart rate, brain activity, and body movements while asleep. For straightforward cases, a home study is available. Home testing collects less information but may be more convenient. For more complete results, a sleep center/lab is also able to administer the study.
How is insomnia treated?
The best choice of treatments for each person depends on the type and cause of insomnia, and may include:
(CBT-i) is recommended for most people with insomnia, as it addresses the causes of chronic insomnia and helps train the brain and body to be able to sleep naturally. It is typically provided by a clinical psychologist board-certified in Behavioral Sleep Medicine, though other clinicians may also have this expertise. It can be provided in-person, via telehealth, or with an app.
Stimulus control, sleep restriction therapy, paradoxical intention, behavioral experiments, relaxation training, cognitive restructuring, and sleep compression are other behavioral and cognitive therapies that may help for certain types of insomnia.
Helpful lifestyle strategies include keeping healthy sleep habits (also called sleep hygiene) and relaxation techniques, though these are typically only helpful for mild sleep problems and not chronic insomnia. Social support, through connecting with other people who have insomnia, can empower people to learn coping strategies.
It is possible that other mental or physical health issues that prevent people from sleeping could be contributing to insomnia. Treating these other health issues can be helpful in addressing the insomnia.
Medications can affect different types of insomnia in different ways, and if used incorrectly, can make sleep difficulties worse. Therefore all sleep medications, including those available without a prescription, should be used with the advice of a sleep specialist.
Prescription medications approved by the FDA for treating insomnia include orexin receptor antagonists, benzodiazepine receptor antagonists, benzodiazepines, melatonin agonists, and heterocyclics. These medications may be helpful if used occasionally. However, if used long-term, some of these medications can become less effective and can be habit forming. Some medications can cause complex sleep behaviors such as sleep walking and increase the risk of accidents.
Some additional medications are prescribed “off-label” to treat insomnia. These medications treat other conditions but have been shown to be effective for insomnia. Not recommended for treating chronic insomnia are over-the-counter medications and supplements. These include melatonin, diphenhydramine, L-tryptophan, and valerian, none of which have been shown to be effective.
Additional Resources
For more information and resources, please check out Diane Macedo’s bestselling book, The Sleep Fix. This book offers readers expert wisdom, cutting edge research, and practical ways to incorporate evidence-based sleep solutions into our busy, everyday lives.
Please also download our free, printable Insomnia Fact Sheet. This is a handy resource to share with friends, family, and medical providers.