The Project Sleep Podcast: Tackling Insomnia
Meet Our Episode Guest

Diane Macedo is an Emmy-Award winning news anchor and correspondent, who struggled with insomnia for years. After developing a tolerance to sleeping pills, Macedo decided to attack the problem as a journalist, pouring through research and interviewing sleep experts from all over the world to get to the bottom of what really keeps us from sleeping—and the various ways to fix it. Now a recovered insomniac, Macedo shares what she learned in her bestselling book, The Sleep Fix. This book offers readers expert wisdom, cutting edge research, and practical ways to incorporate evidence-based sleep solutions into our busy, everyday lives. Macedo is also a member of Project Sleep’s Expert Advisory Board.
This broadcast was originally recorded in March 2023, during the annual Sleep In event. Learn more about the Sleep In here: project-sleep.com/sleepin/
More About The Sleep Fix
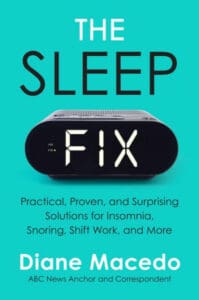
From renowned ABC News anchor/correspondent and former insomniac Diane Macedo, comes a practical, user-friendly guide to getting better sleep. The Sleep Fix flips the switch on common advice, illuminating the reporter’s relentless search for how to get a good night’s sleep and the surprising, scientific, and practical solutions she found along the way.
Learn more at The Sleep Fix Method.
The Project Sleep Podcast
“Tackling Insomnia with Diane Macedo” Transcription
(Sleep Insights Series Episode 10)
Julie Flygare, JD is the President & CEO of Project Sleep, a leading narcolepsy advocate, speaker, award-winning author, and Stanford Medicine X ePatient Scholar diagnosed with narcolepsy and cataplexy in 2007. She received her B.A. from Brown University in 2005 and her J.D. from Boston College Law School in 2009.
Diane Macedo is an Emmy-Award winning news anchor and correspondent, who struggled with insomnia for years. After developing a tolerance to sleeping pills, Macedo decided to attack the problem as a journalist, pouring through research and interviewing sleep experts from all over the world to get to the bottom of what really keeps us from sleeping—and the various ways to fix it. Now a recovered insomniac, Macedo shares what she learned in her bestselling book, “The Sleep Fix.” This book offers readers expert wisdom, cutting edge research, and practical ways to incorporate evidence-based sleep solutions into our busy, everyday lives. Macedo is also a member of Project Sleep’s Expert Advisory Board.
The Sleep Insights Series invites listeners to learn about this amazing adventure we take every night called sleep. Through these insightful discussions, we examine sleep, and our societies beliefs about sleep, from a variety of angles. We hope you’ll learn some cool new facts and analogies that you can use to help us raise awareness about this under-appreciated one third of our lives. This is a written transcription of the podcast “Tackling Insomnia with Diane Macedo” (Sleep Insights Series Episode 10) from Project Sleep. Transcription provided by Mirela Starlight.
Project Sleep is a 501(c)3 Nonprofit Organization, dedicated to raising awareness and advocating for sleep health, sleep equity and sleep disorders.
All guests and speakers express their own opinions. While medical diagnoses and treatment options are discussed for educational purposes, this information should not be taken as medical advice. Each person’s experience is so unique, which is why it’s so important to always consult your own medical team when making decisions about your own health.
This broadcast was originally recorded in March 2023, during the annual Sleep In event.
Julie in intro: Today we’re gonna hear from Diane Macedo, an emmy-award winning news anchor and correspondent, and the best-selling author of “The Sleep Fix”. We’re gonna talk about all things insomnia, and how to incorporate the evidence-based solutions from her book into our busy lives.
Julie: Hello everybody! I’m here with Diane Macedo, hi Diane!
Diane: Hello!
Julie: And we’re so excited and grateful for you to spend some time with us, and if you guys are not familiar with Diane Macedo and her amazing book, “The Sleep Fix“, then you’re in for a big treat today. Well let’s see, how did we meet? I think it’s through Emma Cooksey, probably, is how we first got in touch. And Diane joined the Project Sleep Expert Advisory Board this fall. And then has been part of our community, and then this morning I was actually on her show. She is an Emmy-award winning news anchor and correspondent, and best-selling author of “The Sleep Fix“. Before we get into some of the sleep stuff, I actually was really interested, seeing an interview with you— that you talked about yourself as a writer first. You know, that you really saw yourself as more of a writer, and so I just— I really resonate with that myself as a writer. So just share a little bit about how you went from becoming a writer to being on TV!
Diane: So I wanted to be a writer. I don’t know that I ever— really was. (laughs) But, that was the goal when I first graduated from Boston College. I had worked at this tiny little community news station. And I had done work in news, so I was always interested in that field. But I just never really thought that that was gonna be— a possibility. You know, a lot of people dream of doing broadcast journalism, but I’m kind of a realist and was thinking, well you know, I can dream about that but let’s talk about what’s really gonna happen. And so I thought I was gonna be a writer. And actually even when I started my first job— real job in news, was um— working in radio. And I was booking guests at the time, but my goal was to write. And so I used to stay late and shadow one of the producers who was so kind to me and kind of took me under her wing a little bit— and taught me how she wrote these scripts for broadcast that the anchors would then come in and read for the radio broadcasts. And I started writing my own scripts, to time— and then leaving them for my boss. And he would critique the writing, and then leave them for me. ‘Cause we worked opposite shifts. And so eventually he said, listen, I know that you want to be a writer and your writing is great, your news judgement is great, but— I really think you need to consider broadcast. You know, you’ve done it before— because again I’d worked at that small news station in Massachusetts. But he said, you know, you really have the voice for it.
Diane: And so, he kind of taught me how to deliver. Instead, he told me, instead of giving me these scripts with your writing, I want you to deliver the newscast and record it as if you’re the anchor, and send me the sound. And so he started critiquing my delivery. And long story short, I was obsessed with American Idol because I’m also a singer in my spare time, and we were working such late hours at that time. And you know the whole crew that I was working with, that was when American Idol was like the biggest show on the planet. And so for fun I started an American Idol pool among my co-workers and so there was just a lot of talk about American Idol. And eventually our radio in Philly, it wanted someone to do an American Idol recap. And so that was kind of my first opportunity on air, aside from my early college days, where he said listen, we need someone to do a recap, they want it to be a little bit snarky, which I am— and so he said, have a little fun with it and see how it goes. You’ll still have to do your normal job. This is something that you’re doing in your free time. And I gladly jumped at the opportunity. And so that was the beginning of my on-air career. I started in radio and then eventually I was put on-air by— I left radio and went to work for— a website where I was editing this website and writing for it, they eventually put me on air for .com. And then that eventually led to me being on-air for television. But it was a sort of long, convoluted, completely unplanned journey. Which is why it’s so funny, people will often reach out and say hey, I wanna do the same thing one day, how do I get there? And I remember being that person, asking the same questions and wanting this, you know, formula, this direct path. And the answer is really there isn’t one. Everybody falls into these careers differently. And that was my unconventional path here.
Julie: Oh yeah, I mean I relate to that so much. (laughs) In many ways, you know I don’t think anyone really ever thinks they’re gonna become a sleep advocate, that certainly wasn’t— (laughs) on my list of goals, growing up. And also, you know, I loved writing in college and then when I went to Boston college for law school, that was me being— taking the practical path, that, you know, loving writing, loving art history wasn’t going to be a profession, so I’ll become a lawyer. And then comes along narcolepsy and pretty soon went back to that love of writing, so. I just think that’s so amazing. And good advice for young people too, that you don’t have to have it all figured out when you’re really young.
Diane: No. Not at all. In fact part of my journey— kind of sad, but was giving a eulogy. I gave my cousins eulogy. And someone who was in the audience heard it, and that was how I got my first job out of college, which was before I went into news, where I worked in PR, you know. These things are— sometimes things just fall into place in a way that doesn’t make sense at the time, but it makes sense later. And it’s kind of funny because I neglected my sleep for so long, throughout the course of my career, working all these crazy schedules, doing all these jobs at the same time, just trying to make it. That the fact that I’m now a sleep author, so many of my friends are like, of all the people to write about sleep, you would’ve been the last person. And I was the last person on my own radar for that too, I never would’ve expected to be here today.
Julie: Yeah. So then how did— how did that all change? (laughs)
Diane: Well, when I started my first broadcast job forced me to go from nightwork, which is what I had been doing, you know my shift would end around midnight, often— to morning work. And now I was going in at 3:30 in the morning. And I’m a natural night owl, which I didn’t know was a thing at the time, you know I’ve always called myself that, and other people have called me that. But I didn’t know that that’s a biological thing! And so, working mornings just— wrecked— my sleep. I would try to go to bed early, but I couldn’t fall asleep at that time, and then waking up at three— you know, 2:30, 3 o’ clock in the morning, just was impossible. I mean, I did it, but I felt absolutely awful. And little by little all these symptoms started appearing. I got really bad acid reflux for the first time in my life. I had not been familiar with that at all. Dry eyes, fogginess of the mind— I had a hard time concentrating. Just all these little things that kind of built up over the years, of working in morning and then later, overnight news. And I hadn’t linked any of it to my sleep, and neither had any of my doctors. I was on all these acid reflux medications, I had done all these other tests and no one could figure out anything else that was wrong. And meanwhile I saw my sleep deteriorating but I kind of just always chocked it up to, oh well I’m just a bad sleeper, that’s just how I am, that’s just how I’m built. Unfortunately I’ve learned that that’s very common for people with insomnia. We kind of just assume, oh I’m just a bad sleeper, and no one thinks of about this as a condition that’s actually treatable. And that you should address. We think of it as something that we have to live with.
Diane: But eventually it got so bad that I couldn’t just ignore it anymore. And so I went to my doctor and you know told her what was going on, and she convinced me to take sleeping pills. I was really hesitant, but she assured me it was fine and to, you know, at least just use it after a string of bad nights. And then I started also down this path of looking for my own sleep solutions, and so I started reading all your typical— articles, TV segments, anything that I saw about sleep, I would read it and I would try it. And you know by the end I had lavender oil on my pillow, and I was taking baths every night, I was doing all of this stuff— swearing off screens, quitting caffeine! And I was just getting worse, and worse, and worse, and worse. And for a while that ambien that my doctor had suggested worked like magic. And the more I started reading about sleep and how doomed I was going to be if I didn’t get those eight hours— recommended eight hours— I started getting more and more worried about my sleep, and I started taking that ambien more and more frequently. And it was like magic for a while, and then one day it was like the magic stopped. I took ambien, and I couldn’t sleep. And so I waited two weeks, and I tried it again, and again. Nothing happened. And when I called my doctor and I told her, her suggestion was, just take more ambien. You know, right now you’re just taking one pill, take two. And I just kind of thought right then and there, this is not gonna be the way forward for me. And at the time I was the overnight news anchor for ABC News, where I am now. And so I went to my producers, and listen, we’re an overnight show, right. People are watching us in the middle of the night, many of them because they can’t sleep. And so I went to my producers and I said listen, I’m setting off on a mission to fix my sleep. Do you want me to document it? And we can air it for our viewers. And they highly encouraged it, because they knew it was something of interest.
Diane: And so I set out on that path to do that, I originally reached out to an expert in insomnia, someone who treated people with CBTI, cognitive behavioral therapy for insomnia, first time I had ever heard that term, by the way. And I reached out to this specialist who— quite frankly was just a pain. I mean she wanted me to talk to lawyers, she wanted to approve the footage before I aired it, which no news organization will ever do, that’s just not how it works. And so I kind of tabled that, and ended up going to this dinner speaking event thing, where the speaker happened to be a sleep doctor, who then happened to be seated next to me, at the dinner. And so we then chatted it up and I kind of told him my story, he ended up saying, you know listen, I’m game. Let’s do this. So I said listen, you can put me through— we’re gonna call it Sleep Boot Camp. I will take any test you want me to take, anything you tell me to do I will do, besides quitting my job. ‘Cause I was so tired of hearing, you know, you can’t work overnights, you can’t work these crazy hours, you can’t work these switch shifts, you can’t— you know, you can’t do these things, that I needed to do for my life— in order to sleep well. I refused to believe that I would have to quit my job to sleep well. So I told him I’ll do whatever you want, bar quitting my job. And he said that’s fine, you don’t have to, we’ll figure it out.
Diane: So we did that. So he gave me a series of at-home tests. I learned at that point that you can test at home for sleep apnea, which I never knew. Tested me for sleep apnea, I did not have sleep apnea. But something tricky happened, where my schedule changed temporarily. I had been asked to do a standby shift for Good Morning America on the very day that he’d sent me home with this machine called a Sleep Profiler which analyses your sleep cycles. And so, whenever that happened, because I was on this nocturnal sleeping schedule, any time my schedule shifted that dramatically, it was like I lost the ability to sleep for weeks. At least that’s how it felt. And I had to just gradually then get my body used to sleeping at night again. And so he said listen, your sleep apnea test is negative, but— your sleep is so fragmented with this change in your schedule that the Sleep Profiler results really aren’t conclusive ’cause you’re not getting consistent cycles of sleep to be analyzed. Now under normal circumstances he would’ve just said, you have insomnia, I’m gonna refer you to CBTI, and that’s that. But because I was shooting this— I wanted to document the full process. And so he said, get yourself back to your normal four or five hours, whatever you normally get— and we’ll do the Sleep Profiler thing again so you can show the results on TV and then we’ll do CBTI. And I said great, but— I am, you know a type A, I really wanted to be prepared and especially now that we were kind of setback in our timeline, I wanted to make sure I was uber prepared for when we were ready to start CBTI. So I started doing all this research, reading books written by insomnia clinicians and sleep clinicians in general, reading sleep textbooks. So I could learn everything I could about CBTI so I knew exactly what I wanted to ask, when we started shooting that part of this whole journey. And I also was trying to get, again, back to my four or five hours as quickly as possible so we could move things along.
Diane: And to my surprise, I ended up fixing my own sleep problems, essentially. By implementing some of these super straight forward, practical techniques, based on CBTI and a few other little things here and there— three, I think it was three and a half weeks later or three weeks later, he analyzed my sleep and I was getting six and a half hours of good quality sleep— in the middle of the day, because I was still working my overnight shift. And he was kind of like listen, (laughs) you don’t— you don’t really need me anymore, whatever you did is working, and just keep doing it and you’ll get yourself a little bit higher maybe than those six and a half hours, if you even need more than that. And you’re good. And so I just kind of started thinking, well why isn’t anybody talking about— this stuff. Because these solutions in many cases, one they were super practical. For the most part. And two, in many cases they were counter to everything that I had learned up until that point and everything that I was doing up until that point! And so I just kind of thought, well why isn’t anybody talking about this stuff? Why is the other stuff everything that I’m reading in all these articles and seeing in all these TV segments. And you know over the course of a few years of interviewing sleep experts and doing, you know, looking at clinical research and talking to the researchers and all this stuff, I realized that essentially I was gonna have to be the person that spread that word. So yeah, after why isn’t anybody talking about all this stuff, I finally decided okay, I need to be the person that does it. So I essentially wrote the book that I wished had existed when I was struggling, hoping that it will help prevent other people from having to go through the same thing that I went through.
Julie: Well, I think that you might be the queen of lifehacks, you know I mean, there’s just so much practical advice in this book and— it made me smile, and laugh and— made me so happy because what we often talk about in narcolepsy is about personalized care. That it’s not the same for everybody, that everyone’s situation is a little different. Medications work differently in different people’s bodies. I often talk about the importance of social support, and how doctors don’t talk at all about that. And you go off with a diagnosis and you think you’re the only one— that you live on an island, but you don’t. There’s other people in your same town that are dealing with the same thing and— how important that is, and I just thought that— your approach to talking about individualization, you know that not everything was gonna be the same and what worked for you might be different for other people, but like— there’s just so many different levels of options that you laid out. And interventions that don’t frustrate you, I thought that that was really cool. Was that just natural, like— I guess through your experience, to realize that if something frustrated you that it wasn’t really gonna be a good solution?
Diane: It was. It originated with my experience, but then what I found— I really wanted to write a book that wasn’t, “Hey, this is what worked for me.” I wanted to make sure that I was talking about things that are sound in science and shown to be effective for the general population, not just, hi I’m this random person who’s feeling better now so let me, you know, pretend that’s enough to give recommendations. So I consulted all these different top clinicians and researchers— to merge the two, because what I also found is what works in a lab doesn’t always work in real life. So when you’re talking to sleep researchers who aren’t clinicians, you often will get different answers on what might help. But then when you talk to the clinicians who treat real people who are trying to put this science into their everyday lives, you sometimes get a really different picture. If you look for example at research about screens, you know you put a bunch of people in a lab, who are healthy sleepers by the way, who don’t suffer from insomnia, let’s say. And you give them screens versus not— and they all you know fall asleep 15 minutes later, after having the screens, you might conclude, oh, screens are bad, tell people no screens and they’ll fall asleep earlier. But if you tell people with insomnia who already have this certain level of sleep anxiety which is contributing to their sleep problems to begin with, to now stop looking at screens before bed, that TV time they were enjoying is probably part of their day where they’re using to unwind, right that’s where they unplug from the day. And relax. And start off that process of getting ready for bed. Now you just removed their one source of relaxation, and they will often replace that with a bunch of things that make them think and worry a lot more about their sleep. So for me that was you know the lavender oil, and all of the yoga and the breathwork, and all of the things that I was doing that are supposed to help you relax, they weren’t helping me relax because I was doing them with the goal of— I am doing breathwork, now let’s see if I can sleep. I am taking this bath, now let’s see if it helps me sleep. And it ends up having the opposite effect.
Diane: And so I— in putting all of this together and joining the research with what the clinicians were saying, I started realizing how some of the things that are generally good for sleep, were actually impeding on my sleep and making it worse. And when I spoke to clinicians about this I started realizing, oh this is what typically happens. To people with insomnia. It’s not just me. And so I really wanted to merge those two worlds and then the world of the patient, right. I’m one patient who had that experience. You bring patient perspective into all of your work, and I think that’s really important, and starting to get other tales from people, which are all featured in the book— you start to realize, you know, I listen to all of these different stories, of my colleague Whit Johnson for example, talking about he tried some app that would broadcast a light on the ceiling and you were supposed to breathe along with this app, and it’s supposed to help you relax. I’m sure there are tons of people who love that app! But for Whit, he was like, I couldn’t for the life of me breathe in rhythm with this light, and then it was making me have panic attacks and then I was— wide awake and more frustrated than before. Music, for example— I talked to this great music researcher, Thomas Dickson. And he does a lot of research in how music helps people with insomnia when used in sort of this strategic way, but he says if you’re a musician though, I don’t recommend this, because musicians listen to music differently. We— I say we because I’m a singer, and so I have this in me— I analyze music when I listen to it, I’m not just listening to it passively. And so if someone like me tries to use music as a sleep tool, I’m actually turning my brain on instead of unwinding because my brain’s like ooh, let’s listen to that, and how about that harmony? So I really wanted to write a book, one where the science was really sound. And where I was bringing in all these perspectives because as you’ve mentioned I love a life hack. There’s something in my brain that loves to look at these problems and say, oh how do we come up with a solution to that? And I applied that here where I kind of took what the science says, I took what clinicians were telling me, I took what patients were telling me, and then I tried to think of my own super-busy life.
Julie: Mm-hmm.
Diane: And think about, okay what are the realistic ways that we can now apply all of this, to come up with some solutions that people will actually be able to do. That don’t include things like, quit your job. Which is what everybody was telling me, or— no screens at night! ‘Cause so many of us have to work late. Or, quit caffeine! When often for insomniacs especially, caffeine can sometimes be a tool, to help you get on a healthy schedule and help get your sleep back on track. So the product of that was “The Sleep Fix”, but I really wrote this book with the help of so many people in the sleep science community, and so rather than view myself as kind of this independent sleep expert, I think of myself more as a megaphone, in many ways, for that combination of the researchers, the clinicians and the patients that all came together to help me put this together.
Julie: Yeah, but bringing that practical aspect I think is just so important and just so unique. We were on Capitol Hill this week, advocating for sleep research and sleep awareness and I actually pulled out your book in one of our meetings as we were talking with a staffer who was having trouble falling asleep and— some of the researchers started talking about some apps that sounded very frustrating and I mentioned your colleague, I think that ended up reading cookbooks?
Diane: Yes, yes! My friend Brad.
Julie: Yeah. That that was something that was relaxing and not too stimulating for his brain. And I think for you it was The Real Housewives, watching the—
Diane: Yeah, yeah. I love Real Housewives and that was a recommendation from my acupuncturist when I was undergoing a lot of fertility issues. And you know she said, what do you do that’s just for you? And everything that I rattled off she was able to tie it back to, you do that for your family, you do that for your husband, you do that for your job, you do whatever. And finally I just said, I got it! I watch Real Housewives, and— it doesn’t help me at work, my husband hates it— you know I really just do it for pleasure. And she said, more of that. And so then I came home and joked with my husband that, you know, doctor said I have to watch more Real Housewives. But, I think the larger point there was these common recommendations of do something boring in order to help yourself sleep, again, if you were just to look at the fact that boredom often facilitates sleep, and I’m not saying there’s a lab research on that but if there was— you might look at that and say, that seems pretty straight forward. But you’re ignoring the other response to boredom, which is often frustration. And frustration is a sleep killer. If you feel super frustrated, that boosts your stress response, your fight or flight response, and now you’re waking up, you’re not winding down. And so if you tell someone to read the phone book to fall asleep, or read a computer manual to fall asleep, or in my friend Brad’s case to fold laundry to fall asleep. If that person’s response to that activity is to feel frustrated, then it often will power them up instead of powering them down. And so, I much prefer saying do something that’s enjoyable and relaxing. And yeah, that might be watching TV. That’s fine. ‘Cause yeah, you’re getting a little bit of blue light from the TV, but the amount of benefit that you’re getting from the ability to unwind, and stop thinking about sleep, and stop worrying about whatever else is on your mind— can often be far more beneficial than whatever small amount of blue light you’re getting from the TV screen, which is you know, 10-15 feet away from your eyes.
Julie: Yeah. I love that you said earlier about working in your profession, it is such a unique perspective in multiple ways. Both probably because I imagine that you know there is kind of a go-go-go culture that you’re in— and then I think that the media does certainly has played a role in somewhat perpetuating misperceptions that sleep isn’t all that important. I think that’s shifting now, you know I really think that we’re seeing more coverage that’s valuing sleep, and so you know I was just kind of curious your perspective on that. Obviously you’re putting together great content, but are you seeing that people are excited to look more into sleep in the media, or what more can we do?
Diane: Yeah, I think— I think there’s been a huge shift. I think Arianna Huffington’s book, “The Sleep Revolution” played a huge role in that, I think Matthew Walkers book, “Why We Sleep” played a huge role in that. But in many ways my book came about as result of that sleep revolution, if you will. Because when all of that started, I was fully invested, but all the conversation centered on how important sleep is! And I agree! Sleep is so important. But I also found that incredibly unhelpful, when my problem wasn’t that I wasn’t prioritizing sleep or I wasn’t spending enough time in bed, my problem was that I couldn’t sleep once I got to bed. And I needed a book about that, and that’s what I couldn’t find. And so you know the way that I look at it, I feel like the Matthew Walkers and Arianna Huffington’s of the world did such a great job of persuading us to go to bed and I still think a lot of people need that, but my book is more aimed at— not convincing people to go to bed, but teaching people how to actually sleep once they get there.
Julie: Yeah. I mean that’s actually part of why I founded Project Sleep, to be sleep health and sleep disorders, bridging that gap. Because I often felt that people were talking about sleep health, but not ever in the same article, talking about sleep disorders as a possibility, yet I thought that probably people that were looking to those tips were, you know, engaging in that material— trying to get their Fitbit so they could track their sleep— those people could be the kind of person that could actually have a sleep disorder, but often sleep disorders were not mentioned or those kind of apps or Fitbit technology were saying like, we don’t diagnose sleep disorders, we don’t go there. So that really bothered me, if we think of one in five people could have a chronic sleep condition in the United States, that’s a big segment of the population that had been I think a little bit ignored in that conversation, which was just so glad that you always think to mention, like, okay what else could be happening with your sleep? It’s not that we’re all just skimping on sleep ’cause we want to.
Diane: 100 percent! And the very first chapter in the book is called Identifying The Problem for exactly that reason. There seems to be this— I’ll call it a myth, that if you’re not getting enough sleep, it must be because you have bad sleep habits. I think there’s been a bit of an overcorrection in certain parts of the sleep world where we’ve gone from shaming people for sleeping, ’cause we thought of it as lazy, or whatever— to now there’s an element of the population that I think succumbs to the opposite school of thought, where if you’re not getting enough sleep, that’s shameful. And if you’re not getting enough sleep it must be because something is wrong with your habits. We talk about sleep hygiene, which is you know sleep environments and sleep habits combined, but we talk about sleep hygiene which makes it sound like if I’m sleeping badly, am I dirty somehow? And it feels really shameful when everyone’s talking about how important sleep is, and you’re the person who’s going to bed and staring at the ceiling. I felt ashamed. And so, I wanted, right at the beginning of the book and in all of the other kind of materials that I’m now trying to put together, I really wanna make it clear that this isn’t your fault. Even if you do have poor sleep habits, it’s probably due to some extenuating circumstances, so why don’t we talk about why that’s hard for you and see if we can address that, right. Instead of telling people to put their phone down, why don’t we talk about why it’s so hard for you to put the phone down. And maybe give you some techniques to make that easier. Maybe address the overlying circumstances that make it difficult to put your phone down, you know things like that. Instead of just— I really wanted to come from a place of information and encouragement and positivity instead of shame. Because I felt very ashamed in my journey. And I think the irony is a lot of what made me feel ashamed is a lot of the information that makes it clear that sleep is important. But those things sometimes you know, as you said, we often treat that as a choice, and it’s not always. There are a lot of people who do wanna prioritize sleep, who do think sleep is important. And yet they can’t find the answers to help themselves actually get enough sleep. So I wanted to give people the ability to see that there are lots of behavioral tools and things you can do at home to improve that, but also to be able to flag the warning signs, which are often not obvious— if you have a sleep disorder that needs to be acknowledged by a medical professional. I wanted people to know that and to learn that and to go get the help they need, because when they do— it’s life changing, you know. And you’re just one of many examples of people who will talk about how much their life changed, after getting a diagnosis and starting to be treated.
Julie: Yeah. Well I was kind of curious a little bit about your book process, as well, just as a fellow author, you know. Was there anything that was surprising to you about writing a book, or— like, even— something that you learned about sleep that was really surprising in your process of writing your book?
Diane: Oh, I could write a whole probably on the answers to that question, but I’ll limit it to one which I found interesting. So the first few drafts of the book, or probably my second draft or so— I gave to my husband and my parents and a few, you know, people close to me. Particularly one, they’re mentioned in the book, so I wanted them to see and approve anything that I said about them. But also just to get their feedback, you know, what do you think? And my mother in reading that draft, that early draft of my book— to your point, to the exact conversation you and I were just talking about, she had always— I knew my mother had sleep problems from a very young age. And I saw it play out throughout all of my childhood, you know. As a teenager you try sneaking in late at night, I would try to sneak in late at night, and my mother would be sitting on the couch, awake. Not because she was waiting for me but because yet again she couldn’t sleep that night. And so, identifying my mother as an insomniac was really easy. But when she read the book she said, you know this thing that you talk about, with restless legs— this section of chapter 1 where I describe restless leg syndrome, she said, I think I have that. And so I asked her a series of questions, and— you know, I’m not a doctor, so I wasn’t going to give her a formal diagnosis. But what she described really sounded like restless leg syndrome to me. And I asked her, did you ever bring this up to your doctor. And she said well yeah, actually. I brought it up a few years ago and then I brought it up again last year or two years ago. And I said what happened? And she said, they scanned my legs for blood clots, didn’t find any blood clots, and sent me home. You know, essentially they gave her a diagnosis of, your legs are fine. Because unfortunately medical doctors are not trained well in sleep, as we know. Very little is taught about sleep in med schools. And so her doctor didn’t even think, that hey— this is a red flag for restless leg syndrome. The symptoms she’s describing. Let me refer her to a sleep specialist or a neurologist. And so my mother learned through reading essentially the first draft of my book that she has restless leg syndrome. Which then caused me to start doing the math because RLS is very hereditary. And I started realizing that all of these things that had chalked up to being fidgety or being tired or whatnot, because I almost always will shake my leg if I have my legs crossed, and especially if I’m tired, especially if I’ve been seated for a long time, or if I’ve been lying at rest for a long time. And— yeah, long story short I did the math and realized, I have RLS too. But I did not know that, even after I had fixed my insomnia, I was sleeping better, I had never connected the dots until I wrote the book and until my mother read that draft and identified herself as having RLS. So that was one of many, many lightbulb moments that kind of not only helped me learn more about sleep but also solidified my own recovery because even though by then I had already started sleeping better, writing the book improved that even further because I got to see all these other little areas that I hadn’t thought about and was able to refine that as well.
Julie: Wow. That’s incredible. And I think also one of my favorite parts about your book was at the end, talking about your husband’s experience and how he thought that this was something that was like, ah! So intrinsic to you that he couldn’t believe that so much had improved. I thought that sort of goes in an interesting way to— how we sort of connect these things to our character, or this is just the way it is and it always maybe is going to be this way, or— and to see that real change. And I don’t know, that was just something that was like really emotional and beautiful, I thought.
Diane: It was funny to me because, when he first said it, he said I just can’t believe it’s not a thing anymore. I didn’t really understand what he was talking about. And it was only when I sat down to write that conclusion of the book, and I thought about it, I realized that when we started dating I was already working a morning news shift. It was kind of right after I had started. And so, he had never known me— not having issues with sleep. So he just always assumed, this is you. And he also knew that my mother has a history of sleep problems, so he just assumed, you inherited these sleep problems from your mother, and that’s it. This is just you, this is how you’re built, this is how life is forever. And I assumed the same for so long. But in my recovery and everything that I had learned about insomnia, I knew that was no longer true. But I never, I don’t think, fully related that to him. So it was only in his experience of kind of reading the draft of the book as well, and then seeing that— I was no longer complaining about sleep, I was no longer doing all these things. I had fixed my insomnia, and then that’s it, sleep was no longer this issue and topic of conversation for me, in terms of complaints. That he just, there was this lightbulb moment where he just realized, oh, this is not a thing anymore. You having trouble sleeping. I had thought that was part of you, forever, and it’s not. So it was just really sweet moment of recognizing that was not only a result of my recovery, but it was also the result of everything that I and as result he learned about sleep through the course of writing the book, made that feel so much more solid. Because now not only had I recovered from this thing, potentially temporarily, but I actually now had the tools available to me and the science behind them to know that even if I do end up having problems again down the road, I know exactly what to do to address them. And so that has made it feel I think much more solid that whatever comes our way, I know how to respond to this, I know what to do. And I think that’s really empowering.
Julie: Yeah. Well it always reminds me too, we’re always evolving. I think, soon after a diagnosis can be very overwhelming for people— I know with narcolepsy— and you kind of get a sense like, is it always gonna be this hard? And I try to reassure people, it does get easier over time, and we get better— you know with narcolepsy I don’t know if it gets better, but we get better at it, in so many ways. So, we always are evolving. And I love the part of your book talking— which is somewhat similar to what you’re saying about— I forget the name of the tool but it’s the thing that puts the— it will change the temperature of your bed, it puts water—
Diane: Oh. There are a few of them. The Chilipad is the one that I got, that my husband bought for me, kind of on a whim. But there are a number of them, the BedJet is one that works through air, I think the Eight Sleep is another— so yeah there are a few of them, but essentially it’s a mattress pad that circulates either water or air through it at the temperature that you deem, and some of them will actually respond, to your body temperature and you know respond in real time. Mine is an old, old version, so you just set it at a temperature, you fill it with water, and it kind of— it’s like always sleeping on the cool side of the pillow, is the best way I can describe it.
Julie: Mm. Well I thought it was interesting, which was the next thing I wanted to ask you about, is how you ended up putting it in storage, I think because of having a kid— and then taking it out. And I was kind of wondering how, you know, being a mom— if that impacts your experience with sleep in any way— and if that could be a future book, because I know obviously kids’ sleep is such a big topic. So, I don’t know if you’re ready to life hack that one. (laughs)
Diane: (laughs) I do wanna delve into it and I now have a four-year-old and a one and a half year old, so I am in the thick of it right now. But, for me I think the kids’ sleep conversation is so interesting because— I made the mistake, even after the experience that I had, because I had fixed my insomnia before getting pregnant with my son. But once he was born, obviously I was waking up a lot overnight, to feed him as an infant, as is completely normal. But he started sleeping through the night. And I was still waking up. And then having a really hard time falling back asleep once I did. And I should’ve recognized these warning signs, but I didn’t. Again, I just dismissed it as, oh, it’s just me now! I got used to waking up with a baby and now I have to somehow learn to get used to not. And it was like two months of this where my son is sleeping through the night and I’m still waking up all night long. And I had attributed, I had learned throughout the course of my own, you know, sleep fix if you will, that temperature was a big factor in causing my overnight wake ups. My body temperature was spiking overnight. And so that mattress pad that you described helped me a lot. I also had like little life hacks if I wasn’t sleeping in my bed, where I used like a gel pad that you actually use for dogs, but it was really helpful—
(Julie laughs)
Diane: —that you know and— so yeah, all of it’s in the book. So I had all of these things right, and then somehow when I became a mom, I put that all out the window. I had moved the Chilipad into storage because we renovated our apartment right before my son was born, and I just never got around to taking it out. And so when I finally did and I put it on my bed, and I laid down to sleep that night and I woke up the next morning, you know I was relieved but at the same time I just felt, what an idiot. You just spent all of this time researching and fixing your sleep problems, and then you didn’t even recognize the fact that what you’ve been suffering from for the last two months wasn’t some normal, my baby is, you know, still a baby and that’s just what I do now experience— you had a relapse of insomnia. And you just have to go back to doing the same things you did before. And so I immediately just reinstated all of the tools that I was already so familiar with, and literally like that I was sleeping well again. And so in a way it was frustrating ’cause it felt like, ugh, idiot, you just went two months without sleeping for no reason. But it also reinstilled my confidence that these things really do work, and that you can relapse for any number of reasons, it’s completely normal— none of us are gonna sleep perfectly for the rest of our lives, sleep expert or not— but at least now I feel like I have the tools to be able to address it, and that just takes the pressure off the whole thing.
Julie: Yeah, that’s a—-
Diane: But I think a lot of moms make that mistake, where they attribute their sleep problems to their children’s sleep problems, and sometimes it’s really hard to disconnect those two and realize, yeah my kid might have sleep problems, but I have a problem too. And if I can address my problem, then now I have so much more mental and physical bandwidth, to be able to give my kids the support they need.
Julie: Well, I’m ready for that next book. I mean I’m not personally because I don’t have kids, but— I feel like I can see a next book in your future about hacking kids’ sleep issues, ’cause— (laughs)
Diane: It’s in the, uh— I won’t say it’s in the works, ’cause it’s not actually in the works, but— it’s in the works up here.
Julie: Yeah.
Diane: Once I find some time to actually do it.
Julie: Yeah. In your book I know that you talk a lot about constructive worry, I think is what you talked about.
Diane: Mm-hmm.
Julie: And I thought that was a really fascinating tool. And I just wanted to have you share a little bit about that with people, so that they can think about that as a possible tool.
Diane: So there’s no quick hack to insomnia, but when people ask me, what did you do? This is usually the first thing I mention. Because it’s so simple, it’s, you know practically free— and it’s so effective. So constructive worriers, I colloquially call it the brain dump. Is just, you take a notebook, you divide a page down the center. On the left hand side you write down anything that’s on your mind, like you’re dumping your brain out onto the page. Anything that— the kind of thing you would think about in bed, make a list. And then on the right hand side you just write the very next step to resolving that issue. And you might not know the ultimate solution. That doesn’t matter, the goal here is not the ultimate solution. Just, what can I do to move this in the right direction? So it might be something as simple as, “I’m gonna call Julie about this because she knows more about this than I am,” so I’ll write call Julie. Or, I’m gonna research this on, you know, X website, because I know they have information about this. Look it up on X. The more specific you can be the better. And once you’re done and you can’t think of anything else that’s on your mind, the exercise is over. You close your notebook, put it in your nightstand and then you know when it’s time to go to bed, you go to bed. If something else you know occurs to you in the middle of the night that you haven’t written down in your notebook you can go ahead and jot it down if you want. And if something occurs to you that you have written down, you already know hey, I’ve processed this, I’ve already figured out what I’m gonna do about it. Nothing I can do about it now, in the middle of the night.
Diane: And when I first read about this technique, which is a technique in cognitive behavioral therapy, I thought, listen, ambien doesn’t put me to sleep anymore but this little to-do list thing is gonna help? But it was so effective and now I know why. One, as you said, so many of us are go, go, go all day long. We’re not really giving ourselves the chance anymore to process that conversation I had earlier in the day or what I think about this interview that I have coming up tomorrow. We used to have kind of built in down time, when you were sitting at a traffic light or something, you would think about these things. Now, we reach for our phones. And so, when you don’t give your brain the chance for that kind of processing of your thoughts and feelings from the day, your brain will have to do it at the first opportunity it gets. And often the first opportunity we give our brains for downtime is when our head hits the pillow. So by doing this exercise before bed, you relieve the need to do that processing in bed. We also often get repetitive thoughts in our sleep, and that’s your brain just reminding you of something. Same way you would remember a phone number if you couldn’t write it down, it’s your brain just saying hey, don’t forget to deal with this issue and this issue and this issue. So if we write them down we already know we don’t need that reminder because we know we wrote it down. The exercise itself also gets you more geared towards solutions instead of problems. So instead of just ruminating on a problem, which we tend to do more at night, this kind of rewires your brain to start thinking, problem? Okay, let’s think about what we’re gonna do about that problem. Instead of just, problem, problem, problem, problem. And all of these things combined, they do something really cool. And that is they kind of do rewire your brain because this isn’t an exercise you have to do forever, clinicians will often recommend doing this every day or every night, two to three weeks, and after that your brain starts to do it automatically. Which is kind of the coolest thing, after a while I realized I didn’t have to do the notebook thing, because that’s just what my brain does now, when I hear a problem, I’m just automatically thinking like, okay what’s the next thing I can do to address that. So now I wasn’t going to bed with this overload of problems, cycling through my brain and giving me racing thoughts instead of sleeping.
Diane: The other part of it is, insomnia often is a deterioration of the connection that you have between your bed and sleep. If you spend enough time frustrated and awake in bed, our brains all have this autopilot feature as I call it, that recognizes patterns in our behavior and prepares for what’s next. So if you go to your favorite restaurant, you might salivate before the food even hits the table. Because your brain recognizes that place and says, oh I know where we are, we’re about to have some awesome food. And it starts to prepare for that automatically. The same thing happens if you spend too much time awake and frustrated in bed. If you— your brain starts to learn that bed is a stressful place where we have to be alert. Instead of being a calm place where we go to feel sleepy. So now as you start to get ready for bed, instead of your brain taking that as a cue to wind down, your brain takes that as a cue to power up your fight or flight response, because you have to go to that place where you’re literally about to, you know, do battle in the mind of your brain. Because all it knows is, you go to bed, and this is the place where we get worked up about things. And so by doing this exercise, it really helps to cement your bed as a place for sleep because your brain starts to learn, oh this is the place where we worry about things and process our thoughts and feelings. Not when my head hits the pillow. And so I love this technique, again you only have to do it for roughly two to three weeks is most recommendations and then you’ll probably notice your brain does it automatically. But I still keep a notebook in my nightstand, and if I have a particularly stressful day, I’ll whip it out. If my husband’s asleep, I’ll go out onto the couch if I need to, just a few short minutes of jotting things down. And I normally find that really helps to relax me and then I go to bed and I can drift off.
Julie: I think it’s great. I think I’ll be trying some of that. Also just ’cause that nice connection that you make between writing down the worrying but then also the next step. I think that’s always so important. So, yeah, I think that’s a great exercise for people to try. And I love the one too about Dr. Grandner mentioning, about standing up while you— I haven’t actually done this though, I know he says it and I think it sounds nice, that, you know use your phone but stand up. And then you have to put your phone down if you wanna lay in bed. I always think that’s really smart of him, but I haven’t tried it yet. I just think your book also just pointed out how there’s been so much focus on that nighttime— you know, using the blue light and screens— but that there’s really such an important issue around getting that morning sunlight, that we need that and how important that is and how that hasn’t really been emphasized as much as, don’t use your screen right before bed. So I was just so glad to see that you highlighted that as well. I was talking about you this week on Capitol Hill, we were with sleep researchers, and they asked a question for you. What kind of sleep research would you like to see be done in the future?
Diane: Ooh, that’s a great question. I’m so bad at these speed questions ’cause I always wanna like sit and analyze and think about it. I mean, for me I think just more needs to be done in linking all of these things together. And I would say definitely a lot more on nutrition and the impact on sleep, because we have a lot of data on the other way around, right, and how lack of sleep can affect your diet and so on. Very little on how food can positively impact sleep. So I think we need more research on that. I think we need more research on CBD for example, I’m asked about it all the time, there’s such little data on it right now. But also just the general understanding of psychology and sleep and how those two things work together. We focus so much on the physical and the biological, that so many people have no idea how their minds are keeping them awake and how the fact that they’re not sleeping is impacting their mental health. And it’s all this really horrible cycle, that if you pull on the right thread, can start to turn in the other direction, and you just get better, and better, and better and better. And so, definitely more work in all of those areas.
Diane: And then just trying to get more, I think, synergy in the sleep community. One of the beautiful things that I found in writing my book was by talking to circadian researchers and insomnia researchers and nutrition researchers and all these things, I started to notice all these connections and put the puzzle pieces together, but I think when you’re working in these areas, and these people are so wonderful and their knowledge is so deep— that I think if someone is there to help bridge the gap between the two, they can find how much one work actually relates to another in so many ways. And one quick example that I’ll give is a connection that I made that isn’t— I haven’t seen talked about anywhere else, which is one of the things that triggers your insomnia response is your fight or flight response. Something called hyper arousal. And among other things, your fight or flight response will dilate your pupils, right it makes your heart beat faster, it increases all of your senses. So that you can see better in the dark, so that you can smell more, so that you can feel more. Right, and nobody ever understood things, or I never understood why— I couldn’t sleep with a sleep mask. But the touch, the sensation, when you are in that insomnia state, anything that touches your skin you are so much more sensitive to it because it increased that sensation, right. Same thing with your eyes, your eyes will dilate to take in more light because your body thinks you’re about to do battle, so it’s trying to see better in the dark. It’s trying to prepare you for that. When you’re trying to sleep, that’s really, really unhelpful, it’s the opposite of what you want. And so I had even sleep doctors essentially call my bluff, as to how light sensitive I am. You know, I would say, if the cable box reboots in the middle of the night, which sometimes the cable company will do, I will wake up. And I had a sleep doctor who knows his stuff, he’s wonderful, essentially say, yeah, you know, what you think it is, but something else is waking you up. And I know now that’s not true, but by talking to then a light researcher, who specializes in the role of light in sleep and a circadian researcher— I got to learning that light doesn’t just impact our circadian response to sleep, light is also immediately alerting. And people take in different amounts of light through their eyelids, so if you can have thicker eyelids than somebody else, and you might end up with a closed eye, take in less light than I do with a closed eye. And because of this insomnia response, you know dilating your pupils, if you are in that state, your eyes are gonna take in a lot more light, even with an open eye, than somebody else who is in their normal kind of relaxed, ready for bed state.
Diane: So if you combine all of these things, you can end up with someone who is a very light sleeper and very light sensitive and as a result can be woken up with the tiniest little light. But you won’t be able to explain that phenomenon, unless you talk to all of these people. And get to know the physical reactions that are happening when you’re in a state of insomnia, to be able to then put it together. And so I was able to finally explain why I needed to get portable black-out blinds and couldn’t just travel with a sleep mask at the time. And all of these other things that I was doing, and why now I can sleep with a sleep mask, no problem. So now I just travel with that instead of the whole big she-bang. But getting that understanding for me was so validating because it helped to explain so many things that even the best sleep researchers and clinicians and whatnot were not able to explain to me. So I feel like if you are able to join these worlds together more, we’ll have so many more explanations and answers and as a result, so many great solutions for these problems that we haven’t even bridged the gap on yet.
Julie: Oh, I mean ever since reading the part about the eyelids, I’ve been doing that test at night, you know—
Diane: Oh yeah!
Julie: (laughs) —if I can, if there’s any difference between putting my hands over my eyes or not. I will say my bedroom is pretty good, actually. I did the test and it seems to be nice and dark at night. At least for my eyelids, (laughs) for however thick they are, or whatever. So, yeah I just think that’s the masterpiece of what you put together in this book, is bringing all those pieces together. I just hope you feel so proud and I’m sure you do hear it from so many people but, you know just thank you, so much— for doing all this, and putting it together— and also, maintaining— a personality in it and a snarky, you know, humorous tone that I think makes it approachable and human and real. So I guess just yeah, thank you for being real and giving real, practical and amazing tips and advice and bringing all these fields together. We just need so much more of that, so I’m just really grateful for all that you’re doing, Diane.
Diane: Well thank you! Thank you for having me on, the book was a true labor of love and I’m continuing to move that forward, so— if anybody wants to learn more I’m @sleepfixmethod on all the social media platforms, and I’m cooking up a lot of other good stuff that I’m not ready to disclose yet but stay tuned for more— and Julie just, so happy to— to be with you and to see the mission that you’ve set forth, as well, ’cause I feel like we have different but also very similar stories and I just love what you’ve done to turn this negative thing in your life into a real positive and become a real force in this world to help others.
Julie: Thank you! Making Boston college proud of their—
Diane: Yeah! Go Eagles!!!
Julie: (laughing) Alright, (laughs) thank you.





